Many individuals experiencing homelessness are also battling serious health conditions such as diabetes, COPD, high blood pressure, mental health and substance use disorders.
The devastating effects of these conditions are compounded by the barriers that homeless individuals often face when accessing healthcare services. Conditions that could be managed with preventative care and/or medication often spiral out of control when left unaddressed.
Research has found that age-related health problems such as cognitive and functional impairments typically occur an much earlier in homeless individuals than the general population.
In fact, research also shows that the average age of death can be over three decades earlier– 42 to 52 years of age, compared to 78, depending on the particular population
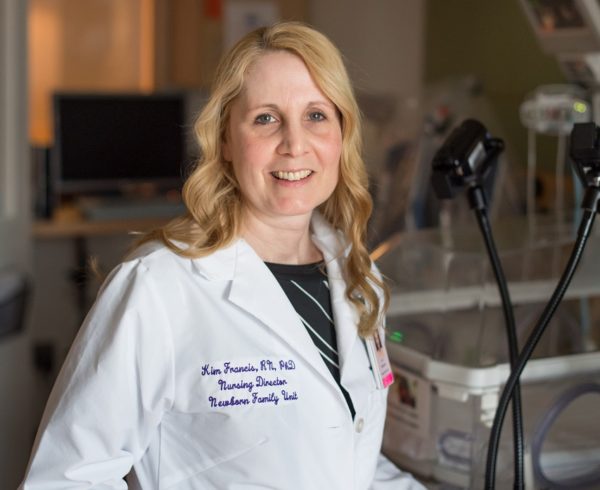
As a social worker, nurse and nurse practitioner in Chicago, Kirsten Dickins, PhD, AM, MSN, FNP-C, has seen the impact of these untreated health conditions firsthand.
“In my perspective, we’re falling short in our capacity to engage folks in a way that better promotes their health,” she says.
The inaugural recipient of the Connell Postdoctoral Fellowship in Nursing Research, Dickins will be working to identify and reduce some of the barriers that homeless individuals experience in accessing and optimally utilizing healthcare services.
The fellowship is a two-year training program established and facilitated by the Yvonne L. Munn Center for Nursing Research at Massachusetts General Hospital with the philanthropic support of the William F. Connell family.
Barriers to Primary Care
The passage of the Affordable Care Act in 2010 expanded Medicaid eligibility criteria, which provided insurance coverage to many previously nonqualifying homeless individuals in the United States. However, many still do not utilize primary care services even when they are available.
This creates barriers to the early detection and management of health conditions and a tendency to overuse emergency departments for medical care, which in turn results in poorer outcomes and higher costs.
Previous research has identified several barriers to primary care that can prevent or discourage homeless individuals from accessing care, including perceptions of discriminatory treatment, feeling stigmatized, prioritizing other needs such as finding food and shelter, a lack of transportation and concerns about the cost of care.
Boosting Access to Primary Care
Dickins is optimistic these barriers can be overcome, however.
“I think from a positive angle, individuals experiencing homeless are invested in their health when given the opportunity to have agency in their healthcare decision making,” she says. “They’ve articulated time and time again—from a research and clinical perspective—that they’re excited about preventative care.”
In a recent study in the Journal of the American Association of Nurse Practitioners, Dickins and a team of investigators identified five elements that could help to increase access to and engagement with care:
- A sense of community
- Mutual patient-provider respect
- Financial assurance
- Access to integrated health services (primary care, mental health and substance use disorder treatment)
- Patient care teams to help in navigating the healthcare system
The study team adds that health centers could champion a culture of respect and dignity through promoting accountability, engaging and supporting staff and partnering with the community.
Ensuring the availability of integrated primary, mental and addiction services are also essential, as homeless individuals face challenges in attending multiple appointments in multiple locations. Nurse practitioners play a central role in providing these primary care services.
Solutions will likely be customized to fit the individual needs of different segments within the homeless population.
The Nursing Connection
“I worked with an advanced practice nurse there, and realized she had the unique biological knowledge and capacity to truly know her patients, and help them to understand their health, facilitate access to medication and emphasize the importance of adherence to treatment,” she explains.
“When I weighed all my options, I was compelled by what the nursing model represented.”
About the Mass General Research Institute
Research at Massachusetts General Hospital is interwoven through more than 30 different departments, centers and institutes. Our research includes fundamental, lab-based science; clinical trials to test new drugs, devices and diagnostic tools; and community and population-based research to improve health outcomes across populations and eliminate disparities in care.
Support our Research
COVID-19 Research at Mass General
Researchers and clinicians at Massachusetts General Hospital Research Institute are mobilizing to develop new strategies to diagnose, treat and prevent COVID-19. Learn more.





Leave a Comment